博文
神奇蘑菇显示对抗抑郁症的功效  精选
精选
||
神奇蘑菇显示对抗抑郁症的功效
诸平
据《英国医学杂志》(BMJ)出版商2024年5月3日提供的消息,神奇蘑菇显示对抗抑郁症的功效(Magic Mushrooms Show Potency Against Depression)。
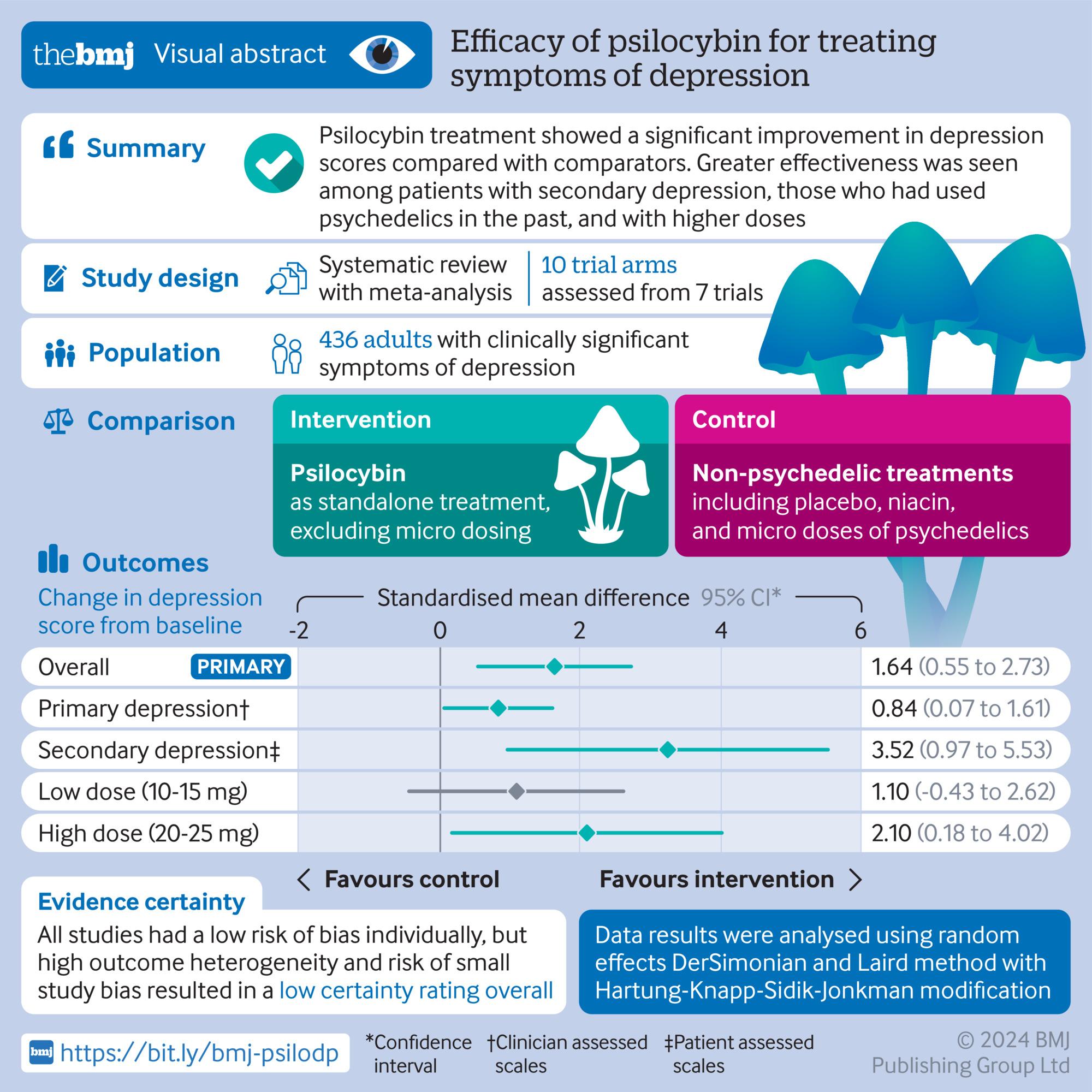
《英国医学杂志》(BMJ)最近的一项研究强调了裸盖菇素(Psilocybin)作为一种有效抗抑郁药(antidepressant)的潜力,与传统对照相比,它显示出抑郁症状的显著改善。研究人员强调需要更详细的研究来充分了解其治疗潜力。相关研究结果于2024年5月1日已经在《英国医学杂志》(BMJ)网站发表——Athina-Marina Metaxa, Mike Clarke. Efficacy of psilocybin for treating symptoms of depression: systematic review and meta-analysis. BMJ, 2024, 385: e078084. DOI: 10.1136/bmj-2023-078084. Published 01 May 2024. https://www.bmj.com/content/385/bmj-2023-078084
专家说,研究结果令人鼓舞,但在提出任何临床建议之前,还需要进一步的证据。《英国医学杂志》(BMJ) 2024年5月1日发表的这项研究表明,迷幻蘑菇(“magic” mushrooms)中的活性成分裸盖菇素(Psilocybin)对抑郁症症状的治疗比对照组更有效,这进一步支持了它作为抗抑郁药的潜力。
抑郁症影响着全球约3亿人,是导致残疾的主要原因。裸盖菇素在服用一到两剂后就有望减轻抑郁症状,而且几乎没有副作用,目前也没有证据表明会导致成瘾。然而,迄今为止发表的研究尚未调查可能调节裸盖菇素作用的因素,包括抑郁症类型、迷幻药(psychedelics)的既往使用、剂量和发表偏差(publication biases)。
研究方法及结果(Study Methodology and Findings)
为了解决这个问题,一组英国研究人员检查了数据库,寻找随机对照试验,将裸盖菇素作为抑郁症症状的治疗方法与安慰剂、烟酸(维生素B)或微量致幻剂(psychedelics)等对照组进行比较。其中包括在实验条件和控制条件下都有心理治疗的研究,以便将裸盖菇素的效果与心理治疗的效果区分开来。他们找到了7项相关的试验进行分析,涉及436名抑郁症患者(52%为女性;90%的白种人)。抑郁得分的变化是用一种叫做赫奇斯g(Hedges’ g)的统计方法来测量的。赫奇斯g为0.2表示影响小,0.5表示影响中等,0.8或更高表示影响大。
与对照治疗相比,裸盖菇素治疗后抑郁评分的变化明显更大,总体赫奇斯g值为1.64,表明裸盖菇素的效果更大。
为解释试验差异而进行的进一步分析表明,继发性抑郁症(与潜在疾病相关)而非原发性抑郁症(用自我报告的量表而不是临床评估的量表进行评估)、年龄较大和以前使用过致幻剂与更大的改善相关。
临床应用的挑战和考虑(Challenges and Considerations for Clinical Use)
研究作者承认,试验之间的高水平差异(异质性)导致支持裸盖菇素强抗抑郁作用的证据的低确定性,并且由于缺乏参与者多样性,研究结果的普遍性受到限制。治疗前的预期以及参与者知道他们正在接受裸盖菇素或安慰剂治疗的程度也未被测量。
此外,在临床试验中,患者在心理治疗师的监督下,在安静的客厅里听着舒缓的音乐,接受裸盖菇素治疗,这在医疗系统中是不太可能实现的。
因此,作者得出结论,尽管本综述的发现对裸盖菇素作为一种有效抗抑郁药的潜力令人鼓舞,但在临床实践中建立裸盖菇素治疗之前,需要解决诸如成本、缺乏监管指南和法律保障等问题。
与该研究无关的研究人员在一篇相关评论中说,这项研究对使用裸盖菇素治疗抑郁症的证据基础做出了重要贡献,但它不能回答几个问题。
例如,他们认为,在收集到更多关于潜在效果调节剂的信息之前,不能为裸盖菇素治疗抑郁症的有效性(在现实世界条件下的表现)提供证据,而实用的临床试验和现实世界的数据可以帮助证明这一点。
此外,关于致幻剂是否可以单独表达抗抑郁活性,而不是通过辅助特定形式的心理治疗,仍有争议。
最后,也许也是最重要的一点,评论作者说,根据所有使用汇总数据的分析,我们无法区分哪些人最有可能从裸盖菇素中受益,哪些人可能反而会出现不良事件。
因此,他们得出结论,这些有希望的发现支持在学术和公共环境中采取谨慎的方法,因为在提出任何关于裸盖菇素治疗用途的临床建议之前,需要更多更好的证据。
上述介绍,仅供参考。欲了解更多信息,敬请注意浏览原文或者相关报道。
Objective To determine the efficacy of psilocybin as an antidepressant compared with placebo or non-psychoactive drugs.
Design Systematic review and meta-analysis.
Data sources Five electronic databases of published literature (Cochrane Central Register of Controlled Trials, Medline, Embase, Science Citation Index and Conference Proceedings Citation Index, and PsycInfo) and four databases of unpublished and international literature (ClinicalTrials.gov, WHO International Clinical Trials Registry Platform, ProQuest Dissertations and Theses Global, and PsycEXTRA), and handsearching of reference lists, conference proceedings, and abstracts.
Data synthesis and study quality Information on potential treatment effect moderators was extracted, including depression type (primary or secondary), previous use of psychedelics, psilocybin dosage, type of outcome measure (clinician rated or self-reported), and personal characteristics (eg, age, sex). Data were synthesised using a random effects meta-analysis model, and observed heterogeneity and the effect of covariates were investigated with subgroup analyses and metaregression. Hedges’ g was used as a measure of treatment effect size, to account for small sample effects and substantial differences between the included studies’ sample sizes. Study quality was appraised using Cochrane’s Risk of Bias 2 tool, and the quality of the aggregated evidence was evaluated using GRADE guidelines.
Eligibility criteria Randomised trials in which psilocybin was administered as a standalone treatment for adults with clinically significant symptoms of depression and change in symptoms was measured using a validated clinician rated or self-report scale. Studies with directive psychotherapy were included if the psychotherapeutic component was present in both experimental and control conditions. Participants with depression regardless of comorbidities (eg, cancer) were eligible.
Results Meta-analysis on 436 participants (228 female participants), average age 36-60 years, from seven of the nine included studies showed a significant benefit of psilocybin (Hedges’ g=1.64, 95% confidence interval (CI) 0.55 to 2.73, P<0.001) on change in depression scores compared with comparator treatment. Subgroup analyses and metaregressions indicated that having secondary depression (Hedges’ g=3.25, 95% CI 0.97 to 5.53), being assessed with self-report depression scales such as the Beck depression inventory (3.25, 0.97 to 5.53), and older age and previous use of psychedelics (metaregression coefficient 0.16, 95% CI 0.08 to 0.24 and 4.2, 1.5 to 6.9, respectively) were correlated with greater improvements in symptoms. All studies had a low risk of bias, but the change from baseline metric was associated with high heterogeneity and a statistically significant risk of small study bias, resulting in a low certainty of evidence rating.
Conclusion Treatment effects of psilocybin were significantly larger among patients with secondary depression, when self-report scales were used to measure symptoms of depression, and when participants had previously used psychedelics. Further research is thus required to delineate the influence of expectancy effects, moderating factors, and treatment delivery on the efficacy of psilocybin as an antidepressant.
https://blog.sciencenet.cn/blog-212210-1432755.html
上一篇:科学家们发现了超越欧姆定律的道路
下一篇:科学家发现新药的惊人效果
