博文
科学家开发出突破性的鼻喷剂,可将老年痴呆症延缓10年以上  精选
精选
||
科学家开发出突破性的鼻喷剂,可将老年痴呆症延缓10年以上
诸平
据美国德州农工大学(Texas A&M University)2024年11月13日提供的消息,科学家开发出突破性的鼻喷剂,可将老年痴呆症延缓10年以上(Scientists Develop Breakthrough Nasal Spray That Could Delay Alzheimer’s by Over a Decade)。
德州农工大学医学学院(Texas A&M University College of Medicine)的研究为将阿尔茨海默病的早期诊断延迟数年提供了有希望的见解。
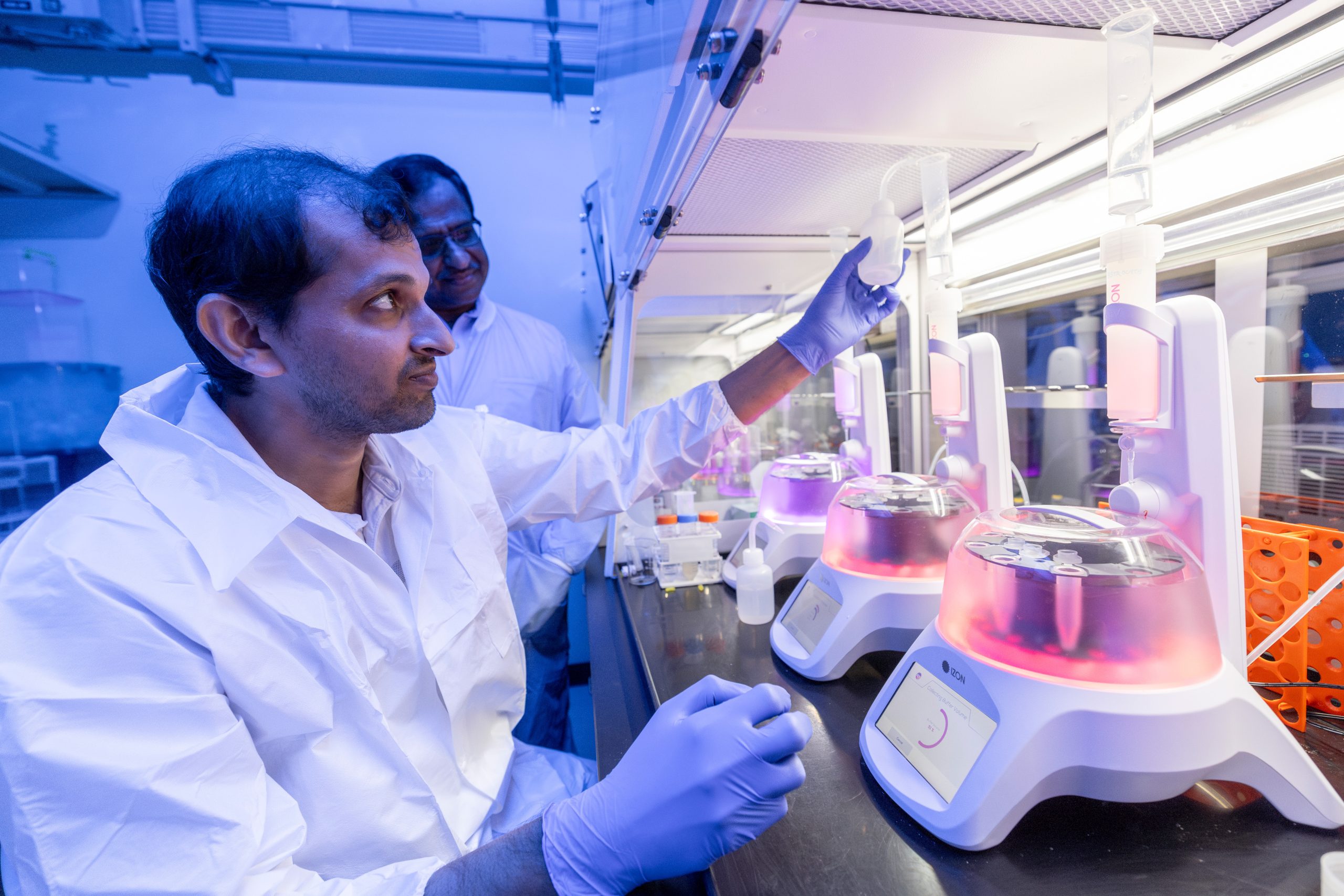
德州农工大学医学院的研究人员最近的一项研究表明,一种新的治疗方法可能会将阿尔茨海默病的进展延缓几年。相关研究结果于2024年11月5日已经在《细胞外囊泡杂志》(Journal of Extracellular Vesicles)网站发表——Leelavathi N. Madhu, Maheedhar Kodali, Raghavendra Upadhya, Shama Rao, Yogish Somayaji, Sahithi Attaluri, Bing Shuai, Maha Kirmani, Shreyan Gupta, Nathaniel Maness, Xiaolan Rao, James J. Cai, Ashok K. Shetty. Extracellular vesicles from human-induced pluripotent stem cell-derived neural stem cells alleviate proinflammatory cascades within disease-associated microglia in Alzheimer’s disease. Journal of Extracellular Vesicles, 5 November 2024, 13(11): e12519. DOI: 10.1002/jev2.12519. First published: 05 November 2024. https://doi.org/10.1002/jev2.12519
参与此项研究的有来自美国德州农工大学健康科学中心(Texas A&M University Health Science Center, Texas, USA)和德州农工大学兽医学院(Texas A&M College of Veterinary Medicine, College Station, Texas, USA)的研究人员。这项研究的重点是开发阿尔茨海默氏症的治疗方案。阿尔茨海默氏症是最常见的痴呆症,也是65岁及以上人群死亡的主要原因,影响着近700万美国人。
研究人员利用鼻腔喷雾剂对慢性神经炎症的非侵入性靶细胞进行治疗,发现大脑中的炎症减少,斑块和蛋白质的积累减少,这些斑块和蛋白质被认为与大脑中神经元的逐渐丧失有关,这是阿尔茨海默氏症的特征。
德州农工大学细胞生物学和遗传学系(Department of Cell Biology and Genetics)杰出教授、再生医学研究所(Institute for Regenerative Medicine)副主任阿肖克·谢蒂博士(Ashok K. Shetty, Ph.D.)说:“这种方法是有效的,因为这些细胞外囊泡携带的物质可以减少大脑中的神经病理变化。”
动物模型的早期试验(Early Testing in Animal Models)
阿肖克·谢蒂与合作者Madhu LN博士以及他们的同事,在阿尔茨海默氏症的早期阶段对动物模型进行了鼻腔喷雾剂治疗。研究人员还发现,小胶质细胞,大脑中的免疫细胞,与鼻内给药的神经干细胞来源的细胞外囊泡结合在一起。
在阿尔茨海默氏症中,小胶质细胞激活引起炎症并清除大脑中与阿尔茨海默氏症相关的斑块。阿肖克·谢蒂说:“这个最初有用的功能随着时间的推移会出现问题。长时间的激活导致它们失去正常功能,并开始损害神经元,导致神经元的进行性损失。”
Madhu LN说,研究结果表明,摄入神经干细胞来源的细胞外囊泡显著改变了小胶质细胞基因表达,减少了多种有害的促炎蛋白,而不影响小胶质细胞继续清除与阿尔茨海默氏症相关的蛋白质积累的能力。
阿肖克·谢蒂已经申请了将神经干细胞衍生的细胞外囊泡应用于鼻内治疗阿尔茨海默氏症和其他神经系统疾病的专利。他说,在他的实验室里进行的这项由美国国家老龄化研究所(National Institute on Aging)资助的研究,已经激发了进一步研究的兴趣,他希望成功的研究可以指明治疗方法,将阿尔茨海默氏症相关的变化和严重的认知问题在最初诊断后推迟10到15年。他说:“我们推进这种治疗阿尔茨海默病的应用之旅才刚刚开始。”
这项研究得到了美国国家老龄化研究所的资助National Institute on Aging (1RF1AG074256-01/AG/NIA NIH HHS/United States and R01AG075440-01/AG/NIA NIH HHS/United States)}。
上述介绍,仅供参考。欲了解更多信息,敬请注意浏览原文或者相关报道。
As current treatments for Alzheimer's disease (AD) lack disease-modifying interventions, novel therapies capable of restraining AD progression and maintaining better brain function have great significance. Anti-inflammatory extracellular vesicles (EVs) derived from human induced pluripotent stem cell (hiPSC)-derived neural stem cells (NSCs) hold promise as a disease-modifying biologic for AD. This study directly addressed this issue by examining the effects of intranasal (IN) administrations of hiPSC-NSC-EVs in 3-month-old 5xFAD mice. IN administered hiPSC-NSC-EVs incorporated into microglia, including plaque-associated microglia, and encountered astrocyte soma and processes in the brain. Single-cell RNA sequencing revealed transcriptomic changes indicative of diminished activation of microglia and astrocytes. Multiple genes linked to disease-associated microglia, NOD-, LRR-, and pyrin domain-containing protein 3 (NLRP3)-inflammasome and interferon-1 (IFN-1) signalling displayed reduced expression in microglia. Adding hiPSC-NSC-EVs to cultured human microglia challenged with amyloid-beta oligomers resulted in similar effects. Astrocytes also displayed reduced expression of genes linked to IFN-1 and interleukin-6 signalling. Furthermore, the modulatory effects of hiPSC-NSC-EVs on microglia in the hippocampus persisted 2 months post-EV treatment without impacting their phagocytosis function. Such effects were evidenced by reductions in microglial clusters and inflammasome complexes, concentrations of mediators, and end products of NLRP3 inflammasome activation, the expression of genes and/or proteins involved in the activation of p38/mitogen-activated protein kinase and IFN-1 signalling, and unaltered phagocytosis function. The extent of astrocyte hypertrophy, amyloid-beta plaques, and p-tau were also reduced in the hippocampus. Such modulatory effects of hiPSC-NSC-EVs also led to better cognitive and mood function. Thus, early hiPSC-NSC-EV intervention in AD can maintain better brain function by reducing adverse neuroinflammatory signalling cascades, amyloid-beta plaque load, and p-tau. These results reflect the first demonstration of the efficacy of hiPSC-NSC-EVs to restrain neuroinflammatory signalling cascades in an AD model by inducing transcriptomic changes in activated microglia and reactive astrocytes.
https://blog.sciencenet.cn/blog-212210-1460187.html
上一篇:代谢酶走向核,为突破性的癌症治疗铺平道路
下一篇:弦理论研究的新难题
