博文
[转载]hLife collection | Antimicrobial resistance (AMR)
||
1. WHO revised bacterial priority pathogens list to encourage global actions to combat AMR
通讯作者:肖永红
The World Health Organization (WHO) has updated its Bacterial Priority Pathogens List (BPPL) for 2024 to combat antimicrobial resistance (AMR), focusing on "One Health" criteria such as treatability, mortality, and resistance trends. The list categorizes pathogens as critical, high, or medium priority, emphasizing the need for new antimicrobials. Notable inclusions are carbapenem-resistant Acinetobacter baumannii (CRAB), carbapenem-resistant Enterobacterales (CRE), and third-generation cephalosporin-resistant Enterobacterales (3GCRE). The AMR crisis, especially with multidrug-resistant gram-negative bacteria, persists, highlighting the urgency for global action, investment, and R&D in diagnostics and therapeutics.

引用:
Ma Y, Chen P, Mo Y, et al. WHO revised bacterial priority pathogens list to encourage global actions to combat AMR. hLife 2024; 2: 607–610.
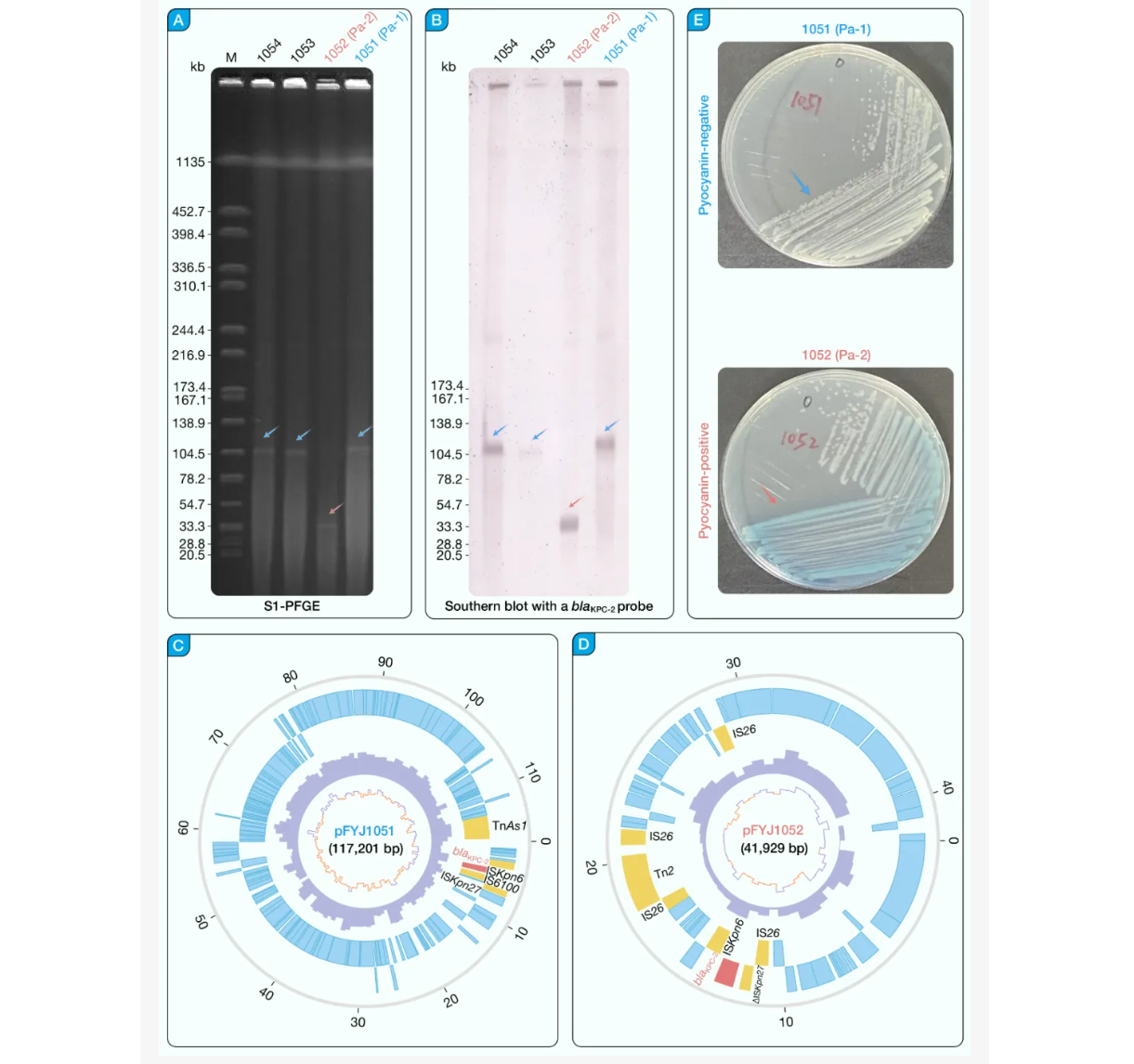
2. Heterogeneity and clinical genomics of blaKPC-2-producing, carbapenem-resistant Pseudomonas aeruginosa
hLife | 揭秘产blaKPC-2的碳青霉烯耐药铜绿假单胞菌的异质性与临床基因组学之谜
通讯作者:黄曼、冯友军
本研究针对临床CRPA感染情况,将分子遗传、比较基因组学与实验动物感染模型结合,较为系统地研究了CRPA的耐药性和毒力分化,指出了CRKP的遗传异质性以及KPC-2耐药性的质粒携带特征,为理解CRPA的复杂播散规律提供了临床基因组学的新视角。
引用:
Huang M, Liu L, Li X, et al. Heterogeneity and clinical genomics of blaKPC-2-producing, carbapenem-resistant Pseudomonas aeruginosa. hLife 2024; 2: 314–319.
hLife | 破解耐药高毒力肺炎克雷伯菌:毒力因子与进化机制揭秘
通讯作者:肖永红
本文系统阐述了耐碳青霉烯类高毒力肺炎克雷伯菌的重要毒力因子和进化整合的多种机制。

引用:
Chen T, Ying L, Xiong L, et al. Understanding carbapenem-resistant hypervirulent Klebsiella pneumoniae: Key virulence factors and evolutionary convergence. hLife 2024; 2: 611–624.
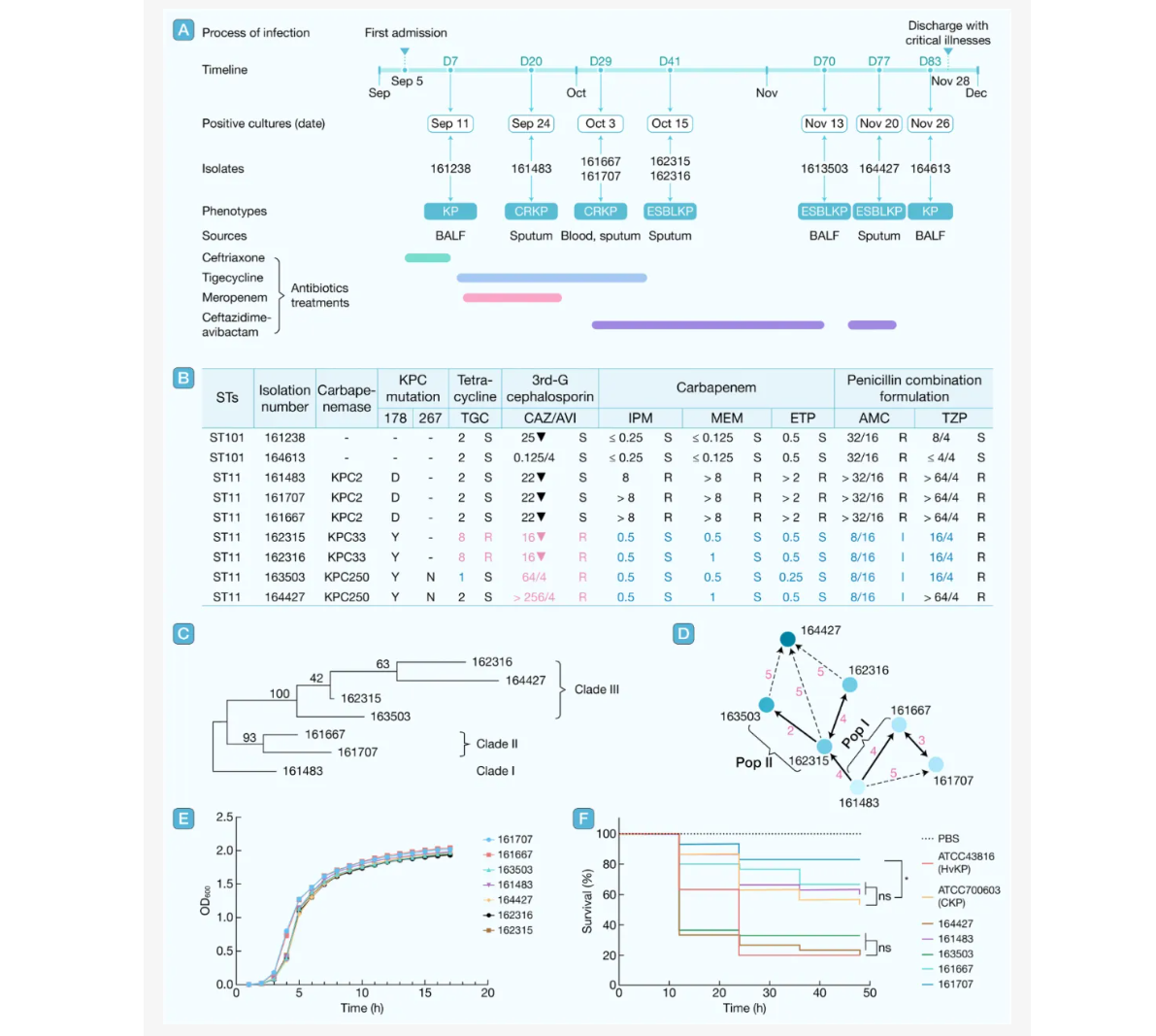
通讯作者:曲久鑫
Nosocomial pathogen carbapenem-resistant Klebsiella pneumoniae (CRKP) poses a heightened risk to public health through carbapenem resistance and virulence convergence, particularly in China's dominant sequence type 11 (ST11) clone. Monoclonal K. pneumoniae exhibits within-host diversity during prolonged infections, with certain variants surviving through adaptation. CRKP strains from the blood of a single patient are heterogeneous in terms of antibiotic susceptibility, capsular polysaccharide production, and mucoviscosity. Intra-host evolution drives novel resistance via cumulative mutations (e.g., the transcriptional regulator gene ramR mutations and the outer membrane porin gene OmpK35 loss). However, the population dynamics and evolution of pathogenic K. pneumoniae within hosts remain poorly characterized. In this study, we analyzed a series of K. pneumoniae strains from a patient enduring persistent infection with K. pneumoniae via whole-genome sequencing (WGS) and revealed their intra-host population dynamics from a quasispecies perspective.
引用:
Li L, Jiang Z, Wang X, et al. Carbapenem-resistant Klebsiella pneumoniae ST11 index from a single strain enhances rapid parallel evolution during persistent infection. hLife 2025; https://doi.org/10.1016/j.hlife.2025.04.007.
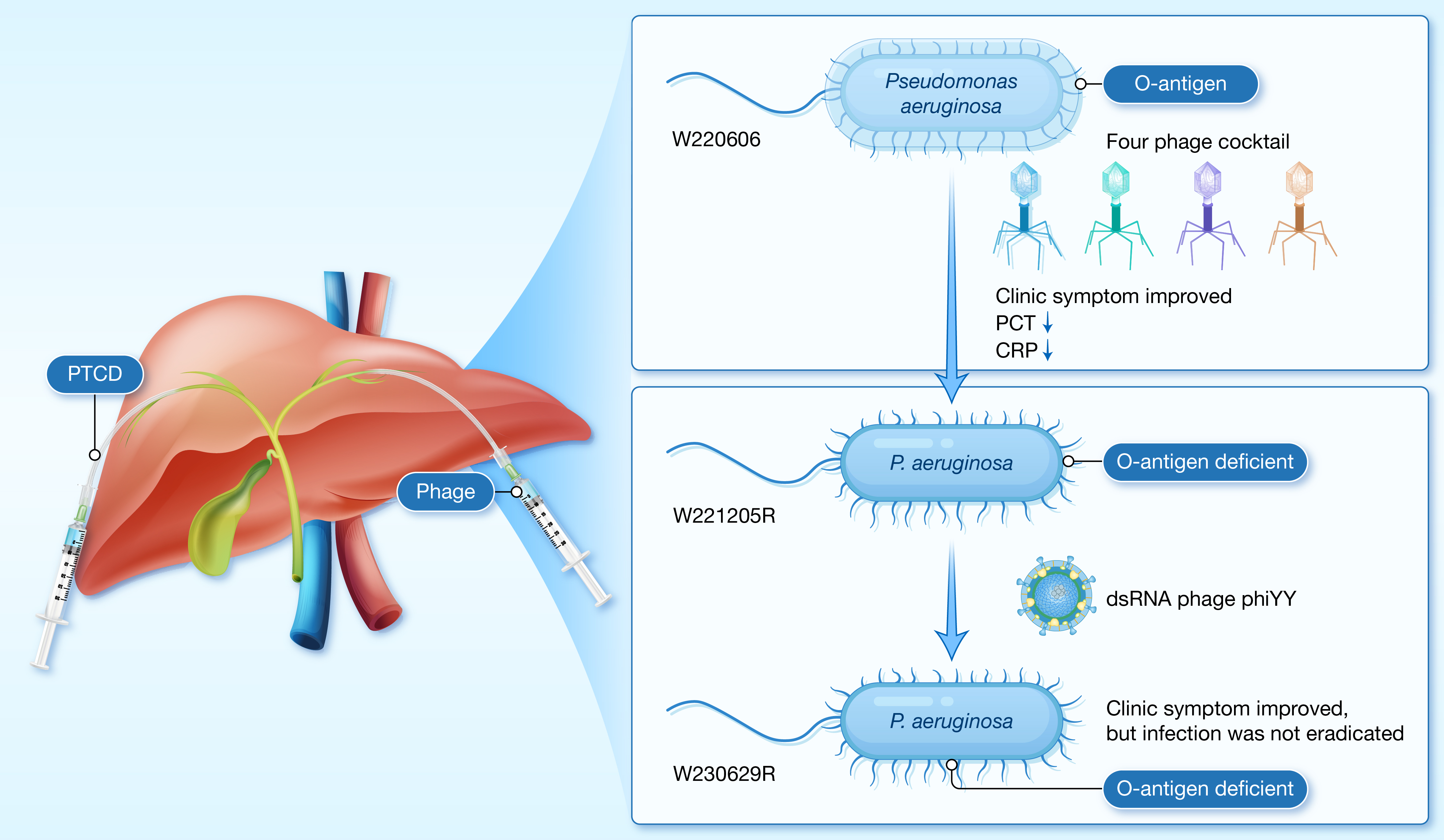
5. Personalized bacteriophage therapy for chronic biliary tract Pseudomonas aeruginosa infections
hLife | 胡必杰与乐率等研究团队合作发现对抗超级细菌的利器!首例超级细菌胆道感染的噬菌体治疗案例!
通讯作者:朱同玉、胡必杰、乐率
本研究首次证实了噬菌体疗法在胆道感染中的安全性和有效性,为治疗提供了新的思路。尽管完全清除感染仍具挑战,但噬菌体疗法在缓解症状和减少细菌载量方面效果显著。未来,研究团队将进一步优化噬菌体治疗策略,以应对细菌耐药性、异质性、生物膜等因素带来的挑战。
引用:
Li N, Li L, He B, et al. Personalized bacteriophage therapy for chronic biliary tract Pseudomonas aeruginosa infections. hLife 2025; 3: 275–283.
通讯作者:王明贵
高耐高毒肺炎克雷伯菌的出现和广泛传播是潜在的公共卫生危机,这类菌株正悄然改变临床感染格局。未来研究和防控策略可聚焦于:基于CRISPR-Cas或毒素-抗毒素系统的去定植研究、针对毒力因子的靶向治疗研究、结合新型分子检测与监测网络的早期预警系统的建立等。只有通过加强基础研究、研发诊断手段、推动多学科协作,才能有效遏制其蔓延,守护临床安全与公共卫生防线。
引用:
Jiang J, Zhang J, Sun Z, et al. Convergence of carbapenem resistance and hypervirulence in Klebsiella pneumoniae: An emerging public health threat. hLife 2025; https://doi.org/10.1016/j.hlife.2025.05.006
hLife | 高毒铜绿假单胞菌的加强版“装备”:共表达同分泌效应蛋白ExoS和ExoU的III型分泌系统
通讯作者:白芳、冯婕
本文揭示了同时携带III型分泌系统效应蛋白ExoS和ExoU的铜绿假单胞菌(exoS+/exoU+)的毒力特征及其演化形成机制。该类型菌株目前已在我国及世界范围内分布,临床上需加强对该类型菌株的监测。
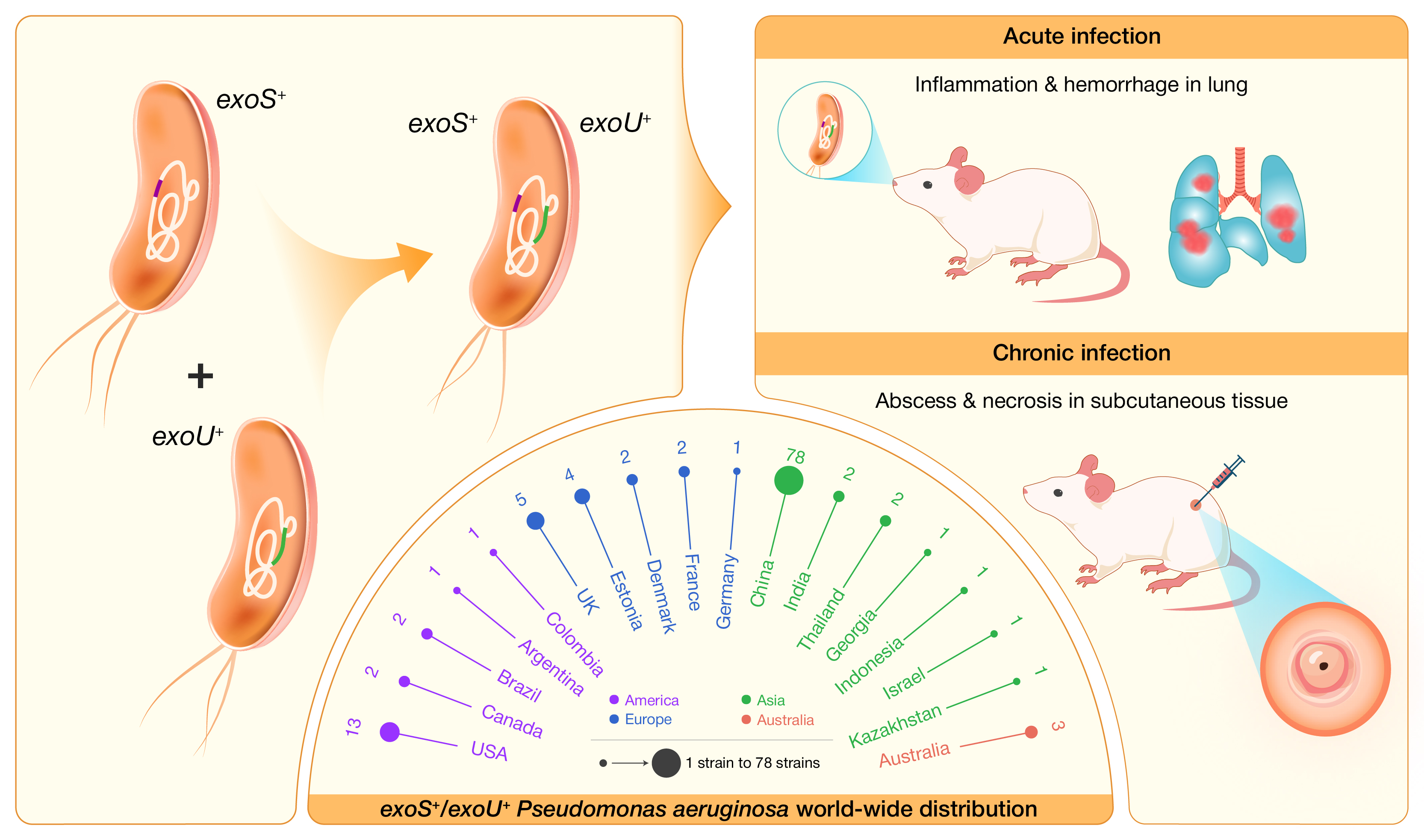
引用:
Song Y, Mu Y Wong NK, et al. Emergence of hypervirulent Pseudomonas aeruginosa pathotypically armedwithco-expressed T3SS effectors ExoS and ExoU. hLife 2023; 1: 44–56.
期刊简介
hLife 由高福院士、董晨院士和Jules A. Hoffmann教授(2011诺奖获得者)领衔,是中国科学院微生物研究所主办,中国生物工程学会,浙江大学陈廷骅大健康学院,西湖大学医学院,上海市免疫治疗创新研究院和广州霍夫曼免疫研究所联合支持,与国际出版商爱思唯尔合作的健康科学领域综合性英文期刊。
hLife 聚焦健康科学领域的前沿进展,旨在促进基础研究与临床应用的融合发展。期刊发表与医学相关各研究领域最新成果,学科领域包括(但不限于)病原生物学、流行病学、生理学、免疫学、结构生物学、疾病监测、肿瘤、药物、疫苗和健康政策等。
hLife是一本金色开放获取期刊,月刊出版;2022年成功入选“中国科技期刊卓越行动计划高起点新刊”;2023年11月正式创刊;2024年5月被DOAJ收录;2024年8月被Scopus收录;2024年10月入选“首都科技期刊卓越行动计划——重点英文科技期刊支持项目”;2025年6月入选北京市科委“2025年度支持高水平国际科技期刊建设-强刊提升”项目;2025年8月入选中国科学引文数据库(CSCD)核心库。
hLife实行高标准与高效率并重的同行评审机制:
投稿至给出“是否送审”决定⏰1天
投稿至给出“首轮审稿”决定⏰28天
投稿至给出“是否录用”决定⏰61天
2026年前hLife接收的稿件免收文章处理费(APC)。
https://www.sciencedirect.com/journal/hlife
https://blog.sciencenet.cn/blog-3552961-1507829.html
上一篇:[转载]hLife | 肺脏与呼吸道黏膜区域免疫十大科学问题
下一篇:[转载]hLife | 巴西探索新模式突破高价药困局,大幅降低癌症与罕见病治疗成本